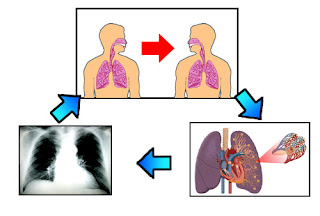
Risk for ineffective airway clearance related to obstruction of the trachea, swelling, bleeding and laryngeal spasms
characterized by:
Maintaining a patent airway to prevent aspiration.
Plan of action / intervention:
1.) Monitor respiratory frequency, depth and breath work.
Rational:
Breathing normally sometimes quickly, but development of respiratory distress is indicative of tracheal compression due to edema or hemorrhage.
2.) Auscultation of breath sounds, record a voice Rhonchi.
Rational:
Rhonchi is indicative of obstruction laryngeal spasm that require rapid evaluation and intervention.
3.) Assess presence of dyspnea, stridor, and cyanosis. Note the sound quality.
Rational:
Indicators of tracheal obstruction / laryngeal spasm requiring immediate evaluation and intervention.
4.) Alert patients to avoid binding on the neck, supporting the head with a pillow.
Rational:
Decrease the likelihood of stress on the injured area for surgery.
5.) Assist in the change of position, deep breathing exercises and cough effectively or as indicated.
Rational:
Maintaining the cleanliness of the airway and evaluation. But the cough is not recommended and can cause severe pain, but it was necessary to clear the airway.
6.) Perform suctioning the mouth and trachea as indicated, note the color and characteristics of the sputum.
Rational:
Edema or pain can impair a patient's ability to issue and clear the airway itself.
7.) Perform reassessment of the regular cast, especially in the posterior.
Rational:
If there is bleeding, bandage the anterior part may seem dry because of blood deposited / collected in region-dependent.
8.) Investigate difficulty swallowing, accumulation of oral secretions.
Rational:
Is indicative of edema / hemorrhage frozen tissue surrounding the area of operation.
9.) Maintain equipment near the patient's tracheostomy.
Rational:
Affected airway can create life-threatening emergency that requires action.
10.) Bone Surgery
Rational:
It might be very necessary for splicing / repair blood vessel bleeding continuously.
characterized by:
- Subjective data: pain swallowing, painful wound.
- Objective data: breathing fast and deep, there is a discharge / thick mucus in the throat, dyspnoe, stridor, cyanosis.
Maintaining a patent airway to prevent aspiration.
Plan of action / intervention:
1.) Monitor respiratory frequency, depth and breath work.
Rational:
Breathing normally sometimes quickly, but development of respiratory distress is indicative of tracheal compression due to edema or hemorrhage.
2.) Auscultation of breath sounds, record a voice Rhonchi.
Rational:
Rhonchi is indicative of obstruction laryngeal spasm that require rapid evaluation and intervention.
3.) Assess presence of dyspnea, stridor, and cyanosis. Note the sound quality.
Rational:
Indicators of tracheal obstruction / laryngeal spasm requiring immediate evaluation and intervention.
4.) Alert patients to avoid binding on the neck, supporting the head with a pillow.
Rational:
Decrease the likelihood of stress on the injured area for surgery.
5.) Assist in the change of position, deep breathing exercises and cough effectively or as indicated.
Rational:
Maintaining the cleanliness of the airway and evaluation. But the cough is not recommended and can cause severe pain, but it was necessary to clear the airway.
6.) Perform suctioning the mouth and trachea as indicated, note the color and characteristics of the sputum.
Rational:
Edema or pain can impair a patient's ability to issue and clear the airway itself.
7.) Perform reassessment of the regular cast, especially in the posterior.
Rational:
If there is bleeding, bandage the anterior part may seem dry because of blood deposited / collected in region-dependent.
8.) Investigate difficulty swallowing, accumulation of oral secretions.
Rational:
Is indicative of edema / hemorrhage frozen tissue surrounding the area of operation.
9.) Maintain equipment near the patient's tracheostomy.
Rational:
Affected airway can create life-threatening emergency that requires action.
10.) Bone Surgery
Rational:
It might be very necessary for splicing / repair blood vessel bleeding continuously.